CurePSP Centers of Care Lean on Each Other to Improve Care of PSP, CBD and MSA
May 21, 2022 By Oscar Sullivan
When Dr. Miriam Sklerov first had the idea for a CurePSP Center of Care at the University of North Carolina Medical Center, she didn’t know where to start. Fortunately for Sklerov, an Assistant Professor of Neurology at UNC, she could take inspiration from the blueprint laid out by her colleague and the medical director of the UNC Movement Disorders Center, Dr. Nina Browner, who had spent many years building their Parkinson’s Foundation Center of Excellence. UNC already offered support groups, educational programs and research for progressive supranuclear palsy (PSP), corticobasal degeneration (CBD), and multiple system atrophy (MSA). Motivated by the new designation from CurePSP, she started a specialty interdisciplinary clinic for people with PSP, CBD and MSA. Today, CurePSP Centers of Care are building on the flagship program, creating new and stronger opportunities for centers to share ideas and resources to make care and support as accessible as possible for patients.
“It’s such a wide open field right now for these diseases,” Sklerov said. “We have an obligation to create that framework and mentor whoever needs help starting these networks.”
Those connections are happening through meetings like the one that took place on April 29, 2022, where CurePSP staff met with representatives from all 28 CurePSP Centers of Care (26 in the United States and 2 in Canada) to reinforce the program’s goals and brainstorm ways for centers to collaborate and grow their network of resources. The CurePSP Centers of Care program, established in 2018, seeks to connect people diagnosed with PSP, CBD, and MSA to the best possible clinical care. The program is at the heart of CurePSP’s mission to raise awareness, build community, improve care and find a cure for PSP, CBD and MSA.
Every Center of Care is tasked with the difficult job of serving patients within a healthcare system that is not designed to comprehensively manage these rare neurological diseases. Given the complex care needs of PSP, CBD and MSA, it makes a multidisciplinary approach, where various experts work together as a team and with other Centers, a necessity. Dr. Jori Fleisher, an Associate Professor at Rush Medical College and CurePSP Center of Care Director, emphasizes palliative care, an integrated approach to treatment that listens to the patient’s needs and adjusts accordingly.
“Palliative care is about wrapping someone in comfort,” Fleisher said. “Until we have a cure, everything that we’re doing is symptom management and enhancing quality of life, and we should be focused on how we will be there with families on this journey.”
Fleisher says that PSP, CBD and MSA are too complicated for any one discipline to treat and support on their own, but when care is done holistically as a team, they become much more manageable. Offering specialized education and resources is central to the mission of the CurePSP Centers of Care program. It is the responsibility of the care team to educate patients and families about palliative care and all of the options available to them. The palliative care model first grew out of the cancer field and has only started to be applied to neurological conditions within the last 40 years, according to Fleisher. There is also the common misconception among providers and patients alike that palliative care is synonymous with hospice, and that hospice means giving up — stigmas that act as barriers to many people with chronic and progressive diseases from obtaining support of a palliative care team.
“You can be in hospice and get great care, and still be connected to the healthcare providers that have been seeing you throughout your journey,” Fleisher said. “Hospice, if anything, doesn’t mean giving up but adding extra layers of support, as well as only being a tiny fraction of the palliative care world.”
Looking ahead, Fleisher says that it is imperative to better educate physicians on palliative care, who have been undertrained on the topic, while also working with hospice specialists to teach them about these rare diseases that they do not regularly see, including how they differ from the more common Parkinson’s disease. Recognizing this, the April convening of the network focused on patient-centered care and discussing ways to work together to enhance the standard of care available for PSP, CBD and MSA.
It doesn’t take long to realize that a multidisciplinary approach is the only way forward, and an idea agreed upon by the two CurePSP Center of Care Directors at the University of Utah. Dr. Paolo M. Moretti and Dr. Guillaume Lamotte have been trying to build a network from scratch in a state with a low population density. Moretti’s CurePSP Center of Care application was accepted in 2019, but then the pandemic hit just as they were ramping up their services. Since then, Moretti and Lamotte have been working hard to grow their network and programs, and while they may not have as many resources as other institutions, Moretti takes pride in what he calls a “virtual multidisciplinary clinic,” where specialists in adjacent departments are just one call away.
“Virtual in the sense that we might be able to set up visits with all of the various specialists more efficiently because we are in contact with them,” Moretti said.
Lamotte combines his dual neurological subspecialities of movement and autonomic disorders in offering a dedicated MSA clinic as part of his CurePSP Center of Care. He has also embraced a collaborative approach, forging relationships with various specialists at the University of Utah such as urologists, gastroenterologists, physical therapists, and social workers to create a “referral pathway” for MSA patients in which they can get the care that they need in a timely manner from clinicians who have a good understanding of the disease.
“The strength of Utah is that we have the different specialties for all of these atypical parkinsonism syndromes,” Lamotte said.
The need and demand is certainly there, according to Moretti, who says that patients will drive as much as five hours, coming in from neighboring states. Moretti is motivated to build the CurePSP Center of Care at the University of Utah into something greater than it was before the pandemic. He has already begun by hiring a health educator as well as a center coordinator to further strengthen their support and care offerings. That process will draw upon the experience of other CurePSP Centers of Care like those led by Sklerov and Fleisher, whose templates incorporate support groups and neuro-palliative care clinics. The paper published by all Centers of Care directors in July 2021, titled “Best Practices in the Clinical Management of Progressive Supranuclear Palsy and Corticobasal Syndrome: A Consensus Statement of the CurePSP Centers of Care,” is another place to start.
Dr. Antoine Duquette, a Neurologist and Assistant Clinical Professor at the University of Montreal, and Director of the CurePSP Center of Care, agrees that local initiatives are critical for support of PSP, CBD and MSA, along with clinical trials and the ultimate goal for these neurodegenerative diseases: a cure. Duquette, who took multidisciplinary inspiration from an atypical parkinsonism clinic at the University of Montreal, looks forward to learning from other Centers of Care to explore models of care based around telehealth and local awareness that could provide unprecedented levels of healthcare accessibility to patients.
“If there is a silver lining to the pandemic, it is how quickly people have adopted telehealth,” Duquette said. “While telehealth is not ideal for initial meetings with a patient, it certainly increases accessibility and promises to improve patient care.”
Perhaps increased awareness will accelerate discovery, which Duquette seems poised to be in the middle of.
“Building this community will help prepare and identify participants for clinical trials,” Duquette said. “Being a CurePSP Center of Care draws patients in and that will also be helpful for future research, so we’re very happy to be a part of this group.”
The CurePSP Center of Care meeting in April is just one important step in the exciting endeavor of strengthening the CurePSP Center of Care network. CurePSP announced a new Collaborative Advances in Research and Enhancing Support (CARES) grant of $80,000 available for Centers of Care, geared towards multi-center projects focused on innovative care delivery, outreach to underserved communities, and education of the medical community. Center of Care directors are eager for further collaboration between experts in the field and CurePSP, expanded care and resources available for PSP, CBD and MSA, and increased awareness of these diseases on a greater scale.
Explore all 28 Centers of care here.
Join our email list
Get the latest news and resources
directly to your inbox.
Get the latest news and resources directly to your inbox.
Sign Up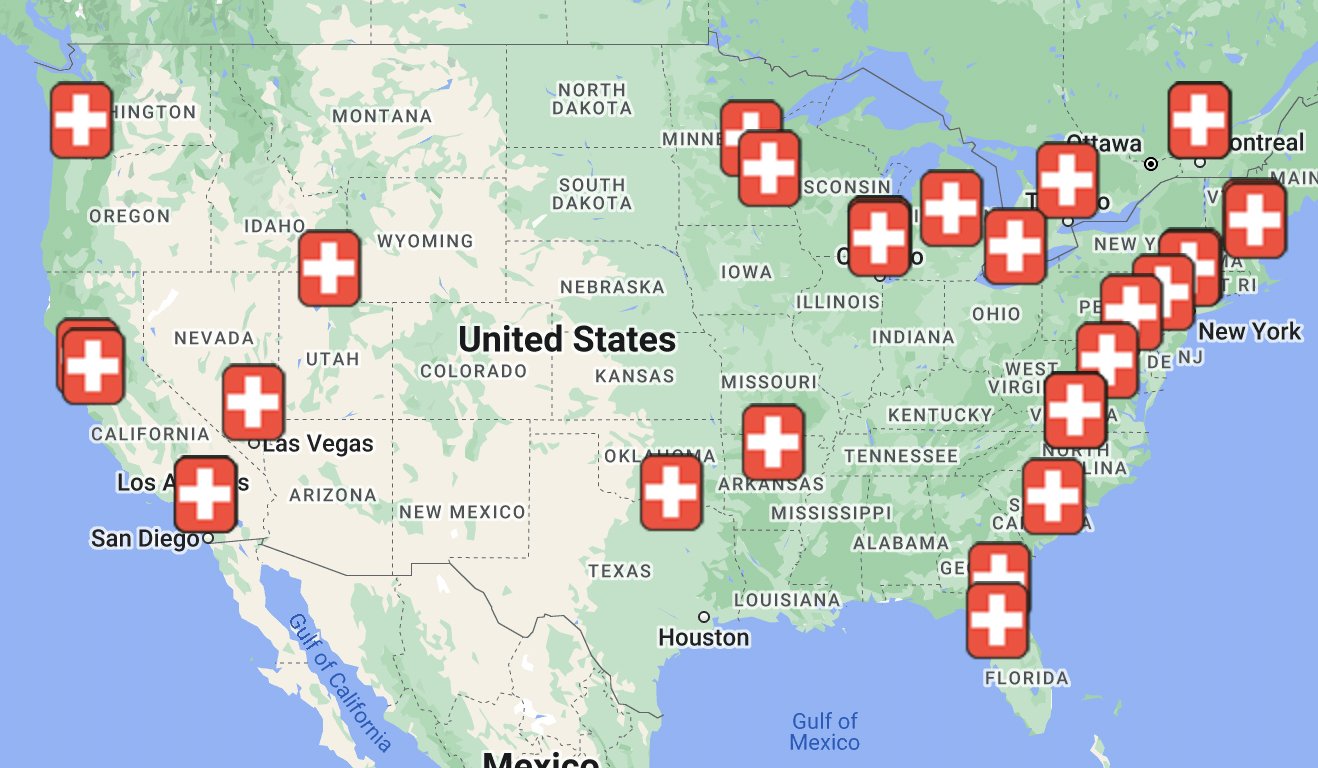
.png)
.png)

